What is hyperemesis gravidarum?

This page contains affiliate links, which means we may earn a small amount of money if a reader clicks through and makes a purchase. All our articles and reviews are written independently by the Netmums editorial team.
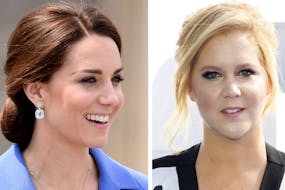
With the Duchess of Cambridge, suffering with hyperemesis gravidarum (HG) in each of her three pregnancies, we look into what this acute pregnancy sickness is and why it's essential to get treatment as soon as possible if – like Kate Middleton – you're suffering. From symptoms to treatments, here's what every mum-to-be needs to know about HG.
What is hyperemesis and why is it different to 'normal' morning sickness?
Most morning sickness eases as a woman's pregnancy progresses – usually between weeks 12 and 16.
It generally puts women off certain foods or causes short bursts of vomiting or waves of nausea – often in the morning, hence the name –and is far from pleasant.
But with HG, the nausea and vomiting is severe – usually with no relief during the afternoon, evening or even at night – and continues into the second and even third trimesters.
FREE NEWBORN NAPPIES
A serious condition that often requires hospital treatment due to dehydration, sufferers usually can't keep any food or drink down, which is why it's important to tell your midwife or doctor as soon as possible if you think you're suffering from HG.
But although HG is much more serious than morning sickness, most women will still go on to have healthy babies – and may not even need to be hospitalised because of it.
What are the signs and symptoms of hyperemesis?
Here's what the NHS lists as the key symptoms of HG:
- prolonged and severe nausea and vomiting – some women report being sick up to 50 times a day
- dehydration – not having enough fluids in your body because you can't keep drinks down; if you're drinking less than 500ml a day, you need to seek help
- ketosis – a serious condition that results in the build-up of acidic chemicals in the blood and urine; ketones are produced when your body breaks down fat, rather than glucose, for energy. (You won't know you're suffering from this without a medical examination – hence why it's important to report any excessive sickness to your midwife or GP)
- weight loss (more than 5% of your body weight)
- low blood pressure (hypotension) when standing (i.e. dizziness).
It can also cause:

- excessive saliva and spitting (ptyalism)
- extremely heightened sense of smell
- headaches and constipation from dehydration
- pressure sores from long periods of time in bed
- episodes of urinary incontinence as a result of vomiting, combined with the pregnancy hormone relaxin.
How common is hyperemesis?
HG affects between 1–3 in 100 women, according to the Royal College of Obstetricians and Gynaecologists (RCOG), making it much rarer than the 1 in 7 who suffer from 'normal' morning sickness.
How long does hyperemesis last?
HG can last through an entire pregnancy, although most severe cases start to calm down by or around the 20-week mark.
Why is it important to get treatment for hyperemesis?
The earlier you can start treatment for HG, the more effective it will be, so don't delay in seeing your midwife or GP.
Treatment is crucial because if you're unable to keep any fluids down you'll quickly become dehydrated. This can in turn lead to weight loss and other significant health risks – both to you and your baby – including:
- Ketosis – as mentioned above, ketosis is a key symptom of HG that can cause kidney damage in you but can also affect your baby's development and growth in the womb. This can be easily detected using a dipstick to test your urine and can be treated using IV fluids to rebalance your ketone levels.
- Deep Vein Thrombosis (DVT) – as HG can cause dehydration, there's an increased risk of deep vein thrombosis, a blood clot in one of the veins in the body. DVT can be fatal if left untreated.
Will hyperemesis harm my baby?
While there is some evidence that your baby is more likely to have a low birth weight if you lost weight with HG, this is not usually dangerously low.
There is no evidence that physically being sick will do any harm to the baby either.
Will I have to go to hospital for treatment?
If you're unable to keep any food or fluids down for 24 hours, are losing weigh or feeling dizzy, contact your doctor straight away. Your doctor will monitor your condition and prescribe treatments that may help control your sickness.
But if your symptoms are severe or worsen, he'll refer you to hospital for treatment – and to check that your symptoms are being caused by HG and not something else.
To do this, the medical team will probably do the following:
- ask what you've had to eat and drink over the last 48 hours
- test your urine (for ketone levels)
- weigh and measure you to assess any weight loss
- take a blood sample
- scan your baby (using ultrasound or internally if it's early on in pregnancy).
If it is HG causing you to be so unwell, you'll probably be admitted as an outpatient so that you can start treatment immediately.
This will happen in the pregnancy assessment unit or on the gynaecology ward and treatment will involve:
- stopping or reducing your food and drink intake until your vomiting stops
- starting intravenous fluids (a drip)
- testing your urine for ketones
- regularly checking your blood pressure and heart rate (because dehydration can lead to low blood pressure and a fast heart rate)
- starting on antiemetic (anti-sickness) medication (such as cyclizine, prochlorperazine or metoclopramide) either in tablet form or through a drip
- receiving a vitamin supplement, either in tablet form or as an injection into your drip
- wearing compression stockings to help blood circulation and prevent thrombosis (a blood clot in the vein).
The good news is that many women with HG improve rapidly each time they are admitted, simply by resting and being put on a drip to replenish lost fluids. This is because dehydration can play a big part in feeling nauseous and exhausted.
Will I have to stay in hospital?
If your symptoms don't improve your doctor may decide to continue your treatment overnight. If this happens you will be admitted to a hospital bed on the gynaecology ward, and will be reassessed the next day.
Is it safe to take antiemetics during pregnancy?
Although you may be fearful of taking medication during your pregnancy, if you are diagnosed with HG and prescribed antiemetic medication, it's because your doctor will believe that the benefits outweigh the risks.
Antiemetics have also moved on dramatically since the tragic thalidomide scandal in the '50s where a prescribed anti-sickness drug (thalidomide) caused severe disabilities in newborn babies.
If your prescribed antiemetic doesn't work then you may have to try a different one. They all work in slightly different ways so it can be trial and error to find the best one for your symptoms.
How else can I treat hyperemesis?
In terms of complementary therapies, there is no proof that acupressure or acupuncture help HG. The RCOG even goes as far as saying that, 'hypnosis should not be recommended to treat HG'.
What you can do to help yourself is:
- ask for help, especially if you have other kids to look after
- take it easy – rest whenever you can; the housework can wait
- eat what you fancy when you can (see more about what to eat below)
- don't feel guilty – you're poorly and it's not your fault
- think positively – easier said than done when you're feeling so dire, but you will feel better (later in pregnancy or once you've given birth)
- talk to someone – it's not unusual to feel anxious, isolated, lonely or even depressed during HG, so make sure you tell someone if you're not coping.
The following organisations can offer support and advice too:
What to eat when you have hyperemesis?
If you can't even keep fluids down then you won't even care about what to eat when you have HG.
However, for some sufferers who feel too nauseous to eat most of the time, hunger can also strike at random times. If you do get hungry, this is your window of opportunity to eat something, advises the UK charity, Pregnancy Sickness Support:
'Missing out on food during your hunger window can bring on a relapse which may see you incapacitated for days afterwards and can make you so nauseous that you throw up on an empty stomach, so it is very important to always have food to hand.
'Try carrying food with you, such as cereal bars, nuts, dried fruit, bread, crackers, peanut butter sandwiches and crisps.'
What causes hyperemesis?
If you've not been pregnant yet and are keen to avoid HG, experts say there's little you can do.
This is because it's not yet known what causes hyperemesis, or why some get it and other's don't.
According to the NHS, some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
These factors are also thought to increase your risk of HG:
- Having HG in a previous pregnancy
- A family history of HG
- Being overweight
- Being a first-time mother
- Carrying twins or triplets
- The presence of trophoblastic disease (an extremely rare condition that involves abnormal growth of cells inside a woman's uterus).
Will I get hyperemesis in my next pregnancy?
If you've had HG before, there's nothing you can do to avoid getting it in future pregnancies, unfortunately. The chances of it happening again are high.
The Duchess of Cambridge is a prime example, having suffered from HG in each of her pregnancies so far.
If you do suffer with HG again in pregnancy, remember to get treatment asap. With the right support and treatment, chances are you'll go on to have a happy, healthy baby, no matter how dreadful it makes you feel along the way.
You may even be able to preempt HG and start medication before symptoms kick in, so talk to your GP when you're planning to try again, or as soon as you find out you're pregnant.
What mums say about hyperemesis
Here's what some of you have said about HG in the forum...
'I used to go through a lot of ice. If I did keep anything down it would have to be really bland like boiled rice, and only drink I could keep down was Volvic strawberry water.'
'Hyperemesis is a very lonely condition as nobody can possibly understand unless you've been there. I was very lucky second time as the hospital were fantastic and wouldn't discharge me until it was completely under control. Several drugs later we hit on Ondonsatron which works with a different part of the brain to other anti-sickness drugs. It was a miracle for me as it finally stopped me throwing up.'
'I ate mashed potato (you can buy bags of little frozen portions of it from supermarkets – just zap in the microwave for a minute. I would have a little piece every hour and I found it really helped.) Sipping cold apple juice through a straw was also tolerable.'
'I found tablets helped to some extent, but only after 23 weeks – not sure why, but it's worth persevering with them. Try taking them on an empty stomach and lying down for a sleep straight after them. Get as much sleep as possible, and get others to deal with housework, etc. You will only feel worse if you don't rest.'
'I've been keeping a diary of what I eat and when I'm sick so I can shove it in the triage nurses face everytime I hit A&E with my sick bucket. But the best advice I was given was by my doctor who pretty much gave me a little flow chart of what I should try to eat, and what I should move onto when I go half an hour without throwing it up. It went like this: ice cubes; ice lolly; sip of water every 5 minutes; table spoon of fresh fruit juice every 5 minutes; a quarter of a breadstick every five minutes; a tiny amount of soup.'
If you're suffering from HG during your pregnancy, get support and advice in the Netmums forum below.
And if you're keen to help those around you understand what you're going through, make sure you show them this checklist of what not to say to someone with HG.