Getting pregnant with IVF
This page contains affiliate links, which means we may earn a small amount of money if a reader clicks through and makes a purchase. All our articles and reviews are written independently by the Netmums editorial team.
Getting pregnant with IVF (or in vitro fertilisation) has a 2-29% success rate depending on your age and the cause of infertility. We look into how this six-step process works, how much it costs as well as the risks associated with this type of fertility treatment.
What is IVF?
IVF stands for in vitro fertilisation. It's one of several techniques that can help couples who are struggling to conceive naturally.
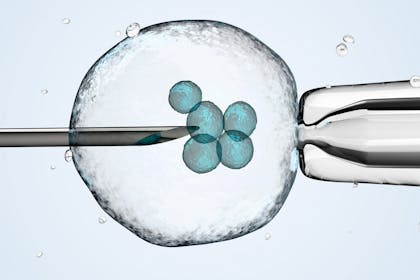
Although it's a complex process, it works by collecting a woman's eggs and manually fertilising them with sperm in a laboratory – so outside the body.
If fertilisation is successful, the egg becomes an embryo and this is then transferred back inside the body, into the woman's womb to grow and develop over the next nine months.
FREE NEWBORN NAPPIES
Who's eligible for IVF in the UK?
If you're struggling to conceive naturally, the first thing to do is see your GP about your options as IVF could be one of them. But, whether it's available on the NHS and therefore free will depend on your age as well as other criteria.
The current NICE (National Institute for Health and Care Excellence) recommendations suggest that you're eligible for IVF on the NHS if:
- you live in England or Wales
- are under the age of 43
- have been trying to get pregnant through regular unprotected sex for two years
- you've already had 12 cycles of artificial insemination.
There are further age-related criteria within these guidelines:
- under 40 – you'll be eligible for three cycles of IVF on the NHS
- 40-42 – you'll be offered one cycle of IVF on the NHS.
Where you live is also key in terms of whether you'll be eligible for IVF, not to mention how many cycles you'll be entitled to, if so.

That's because the final decision is made locally – by NHS clinical commissioning groups (CCGs) – rather than nationally.
CCG criteria can be even stricter than the NICE guidelines. For instance, to be eligible for IVF on the NHS they may require you to:
- not have any children already, from both your current and any previous relationships
- be a healthy weight
- not smoke
- fall into a narrower age range as some CCGs only fund treatment for women under 35.
Even if you meet your CCG's criteria, you may only be offered one IVF cycle, rather than the expected three (as recommended by the NICE guidelines). In fact, the Guardian recently reported that as many as 80% of 'eligible' couples don't receive three cycles.
Just recently the BBC's Victoria Derbyshire programme reported that despite NICE guidelines recommending IVF for women up to the age of 42, 80% of areas in England are failing to do this.
The Royal College of Obstetricians and Gynaecologists (RCOG) blames 'inadequate government funding'.
If you're not eligible for free IVF you may have to have it done privately, which will be expensive. Latest figures (2016) show that approximately 59% of UK IVF cycles were funded privately.
How much does it cost?
If you have to pay for IVF it'll cost between £3-5000 per cycle.
However, there could also be additional costs such as your initial consultation, extra appointments, additional counselling and paying to store and freeze embryos.
Make sure you know what's included from the start.
How does IVF work?
There are usually six key steps in the IVF process. These include:
1 Suppressing your cycle
In order to make your fertility medication work, you'll be given medication to suppress your natural cycle. This will be done by nasal spray or injection, which you'll do daily for two weeks.
2 Increasing your egg supply
Daily hormone injections are required to boost your egg production. The more eggs you produce, the more that can be collected and hopefully fertilised, increasing your chance of success.
This stage takes another 10-12 days.
3 Checking your progress
You'll have appointments to monitor things. This may include blood tests, scans and further hormone injections.
4 Collecting your eggs
You'll have a minor procedure to collect your eggs ready for fertilisation. This takes up to 20 minutes.
5 Fertilising the eggs
Your eggs will be mixed or injected with your chosen sperm in a laboratory. Any that become fertilised are now embryos and those considered 'the best' will be transferred back into your womb in the next step.
6 Transferring the embryos
The embryos are put back into your womb using a thin tube called a catheter. Your doctor may describe this procedure as similar to having a cervical smear test – it's not painful and shouldn't require sedation. This will either happen 2-3 days after their development (known as a cleavage transfer) or 4-5 days after development (known as a blastocyst transfer).
The Human Fertilisation and Embryology Authority (HFEA) says that 'in the UK, roughly half of women have a cleavage stage transfer and the other half have a blastocyst transfer.'
How long does it take to get pregnant with IVF?
Once you've had your embryos transferred, you'll be advised to wait around two weeks before taking a pregnancy test to see if IVF has worked.
This final phase of IVF is known as the two-week wait – a period of immense anxiety as you wonder whether or not it has worked.
This two-week wait is often described as the hardest part of IVF treatment.
What happens next?
If you take a pregnancy test or have a blood test and it's positive, you'll have an ultrasound scan to check the pregnancy is developing as it should. Then you'll follow normal antenatal care given to all mums-to-be.
If it's not successful you'll be referred back to your specialist to discuss your options.
What's the success rate for first time IVF?
As well as what's causing your infertility, age is a significant factor for how successful IVF will be.
Latest statistics show that the younger you are when you have this particular fertility treatment, the more likely it'll be to work. However, it's important to be aware that there's still a significant chance that it won't.
According to the Human Fertilisation and Embryo Authority's (HFEA) Fertility Trends Report 2014-2016, the percentage of IVF treatments that resulted in a live birth ranged from 2% up to 29% depending on age.
The breakdown, according to specific age groups, was as follows:
- 29% – for women under 35
- 23% – for women aged 35 to 37
- 15% – for women aged 38 to 39
- 9% – for women aged 40 to 42
- 3% – for women aged 43 to 44
- 2% – for women aged over 44
Will IVF mean I have twins or multiples?
Your chances of having twins or multiples babies is more likely if you conceive by IVF. However, it's a lot less likely than it used to be.
In 2007, the HFEA launched its 'One at a Time' campaign to tackle the high multiple birth rate following IVF.
At the time one in four births were multiple births – 20 times higher than natural conception. This was because it was common practice to transfer more than one embryo (at step six of the IVF process above).
As multiple pregnancies and births are riskier for a mother and her babies, the campaign set out to reduce the multiple birth rate from 24% down to 10% – and it's working thanks to a change in practice regarding how many embryos are transferred.
According to the HFEA:
'If you have more than one good quality embryo available, it’s now best practice for most women to have only one embryo put back in the womb and freeze the others (called an elective single embryo transfer or eSET).
'This is to reduce the chance of you having a multiple birth, which can pose serious risks to the health of both mum and babies, including babies that are more likely to be premature or of low birth weight.'
What's interesting is that transferring one rather than two or more embryos hasn't impacted birth rates.
The HFEA confirms this on its website:
'For most women having IVF, transferring one embryo is just as successful as having a double embryo transfer and your chance of having a multiple pregnancy is much lower.'
Will IVF affect my baby's future health?
The first IVF baby, Louise Brown, was born in 1978 so it's still impossible to know the long-term effects as she's only just in her 40s.
There is some research that suggests babies born through fertility treatment are at greater risk of:
- prematurity
- low birth weight and stillbirths
- heart disease
- high blood pressure
- male fertility problems.
However, research is ongoing and any findings so far have come from fairly small studies only.
Does IVF increase your chances of postnatal depression?
US research has found that there is a slight increase in your risk of postnatal depression if you've had fertility treatment such as IVF.
The study that was conducted in 2011 looked into 60 new mothers who were treated at an infertility treatment centre and had conceived by IVF.
The results found 25% of them had postnatal depression – the majority of whom had mild symptoms. However, the results also found that birth method such as having a C-section also contributed to this increase in PND.
More recently in 2015, Danish research on a larger scale found that IVF increases your chance of depression but only if it is successful and you go on to have a baby.
The study examined data on 41,000 Danish women who received a fertility treatment. It discovered that women who gave birth after IVF were five times more likely to get depression than those who had IVF but were unsuccessful in getting pregnant.
Associate Professor Lone Schmidt, MD, DMSci, PhD from the Department of Public Health, University of Copenhagen explains the findings:
'Infertility affects one in four to six couples who are trying to conceive, and our research sheds light on a little-known field.
'By focusing on the link between having a child after undergoing fertility treatment and the risk of depression, our research can give professionals useful tools in the form of advice and how to handle a pregnancy before and after birth.
'In addition, the findings are important in relation to couples who are thinking about starting fertility treatment. It can be a tough process, and our findings show there is not a greater risk of depression if the treatment is unsuccessful.'
If you have a multiple birth as a result of having IVF, you'll also have a raised risk of getting PND.
According to Twins Trust:
'Mothers of multiples are at a higher risk of experiencing PND – approximately 1 in 5 mothers of twins and triplets are diagnosed by their health professional as suffering from postnatal depression.'
For any concerns about postnatal depression, talk to your fertility specialist, GP, counsellor or midwife and make sure your partner is aware of this risk and aware of the signs.
Who does IVF work for?
IVF helps couples who can't conceive naturally for all kinds of reasons. These could include:
- blocked or damaged fallopian tubes
- male infertility including decreased sperm count or sperm motility
- ovulation disorders, premature ovarian failure, uterine fibroids
- women who have had their fallopian tubes removed
- individuals with a genetic disorder
- unexplained infertility (which affects 32% of couples).
Who does IVF not work for?
As IVF has a relatively low success rate, it won't be recommended to you if:
- you're overweight or obese
- you're over the age of 43
- you're a smoker
- you can have ovulation problems treated with medication
- you're at risk of early menopause.
What are the side effects of IVF?
There are both mental and physical side effects of IVF.
Mentally it can be an emotional process that can put a strain on even the strongest relationship. Counselling or having someone to talk to can help enormously.
There are also a number of health risks associated with treatment.
According to the NHS, these can include:
- side effects from the medications used during treatment, such as hot flushes and headaches
- multiple births (such as twins or triplets) – this doesn't sound like a bad thing but being pregnant with more than one baby increases the risk of complications
- an ectopic pregnancy – where the embryo implants in the fallopian tubes, rather than in the womb
- ovarian hyperstimulation syndrome (OHSS) – where too many eggs develop in the ovaries.




